What looks like “easy money” on the surface, is much like an iceberg with 90% of its mass comprised of liabilities below the surface. There is a lot more to embryo storage than feeding liquid nitrogen to a storage tank.
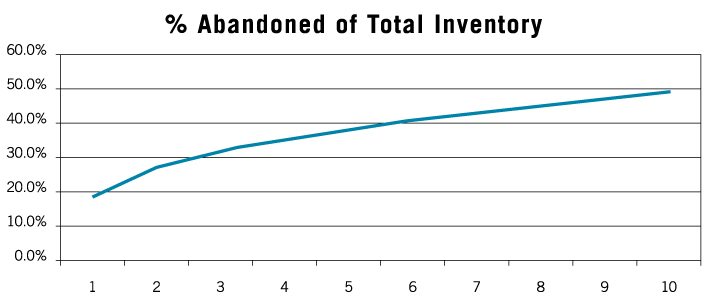
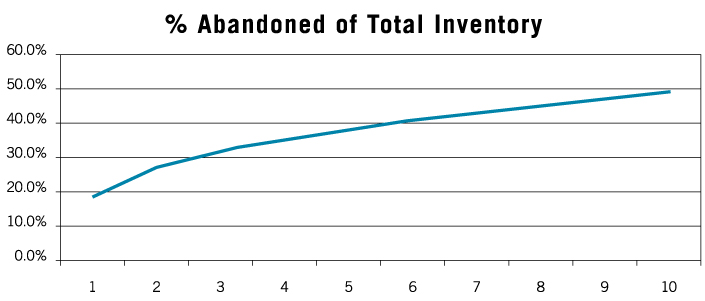
The ultimate truth is that embryo storage results in abandoned embryos, this is true for any IVF center, cryobank, or embryology laboratory. The rate at which embryos become abandoned occurs faster in clinics that don’t have the protocols and dedicated staff to stay on top of the business.
In today’s busy, transient society, simply keeping track of patients for two or more years post-treatment is a difficult task. This is actually even truer for the growing number of oncology patients who are banking sperm, embryos, oocytes, or ovarian tissue and who may store those tissues for 10-30 years.
The bottom line is embryos and gametes turn from assets to liabilities every day across the country. What was once perceived as a revenue stream quickly turns into a liability when no one is watching, especially when abandoned specimens are not dealt with accurately, consistently, and timely. Read more below about the principles of Embryonomics, or feel free to call us if you have questions: 651-478-5603.
THE MYTH is that tanks fail.
THE FACT is people fail. That is not to say there are no documented tank failures, however, the majority of tank failures are actually protocol failures. This is true for both storage and shipping tanks. Staff who are tasked with storage tank inspections in addition to a busy lab schedule can overlook procedures or miss warning signs of tank problems. And maintaining a shipping tank fleet, with proper protocols, to prevent failures requires concentration on the details. Problems occur when clinic staff is not appropriately trained in tank maintenance and validation. Last-minute shipments or poor planning result in staff breaking protocol and not properly preparing tanks for shipment. Storage tank maintenance and shipping should be left to those that have dedicated staff whose only job is to focus on cryostorage and safe shipping, with protocols in place to maintain the absolute safest process available.
THE MYTH is that when a physician retires and closes a practice they’ll just send out letters to all patients to transfer their embryos to another facility.
THE FACT is that even with a six-month window and multiple mailings and phone calls, few clinics have better than a 50% response rate. This leaves your facility with the other 50%. This non-responsive 50% are the patients you must now deal with and in a short period of time. These are now abandoned embryos and a real liability.
THE MYTH is that when a clinic closes, they’ll sell the storage accounts to a cryobank.
THE FACT is most closures result in the closing facility writing a check to the cryobank to accept the whole set of accounts. The fact is that patients who are still actively attempting to build their families will respond and move their embryos to another clinic. What is left then are the non-active patients and in this group, the number of abandoned/non-responsive patients will greatly outnumber the responsive accounts. The physician now must deal with these embryos and their owners. How this liability is handled is highly dependent on the consents/cryostorage agreements that have been in place during the clinic’s operations, the physician’s own tolerance of risk, and in some cases, state laws and ethical positions of multiple organizations. The safest way out of this scenario is generally a paid assignment of the accounts to a professional cryostorage facility. But it isn’t the cheapest.
THE MYTH is that if a clinic keeps possession of the embryos the patients are more likely to complete future cycles at their clinic.
THE FACT is the decision of whether a patient continues to cycle at one clinic is simply dependent on their experience and satisfaction. The current location of their embryos is not a factor in those decisions. The vast majority of embryos which come into Reprotech for storage, if used in a later cycle, go back to the original clinic. Patients who want to switch clinics will do so, regardless of where their embryos are stored. The lab staff is taken away from other duties to instead focus and spend time on receiving, packing, and sending out tanks. Doing so on a patient-by-patient basis is very inefficient compared to monthly bulk shipments to and from a professional cryostorage facility.
THE MYTH is that a clinic’s consents/agreements will protect them.
THE FACT is that most clinics’ consents/agreements will not protect them. Most clinics and laboratories have not properly revised their storage agreements to accurately keep up with changes in case law and technology, leaving them vulnerable to legal disputes. Death, divorce, or separation of couples or individuals can pull your clinic into a lawsuit, even when you think you dotted all the “i”s and crossed all of the “t”s. We all know of lawsuits that have been settled quietly and effectively, but we also know of colleagues who have appeared on the front page of the newspaper or the six o’clock news. There’s no protection from bad press, and it is hard to recover from.
THE MYTH is that when the tanks in the lab fill up, we can add another tank.
THE FACT is very few laboratories were designed and built to accommodate the number of embryos they are now storing; likewise, few inventory management programs are capable of keeping up with the extra demands of large embryo storage especially with the added regulations placed on clinics by the FDA and state oversight. Adequate expansion of alarm systems, as well as floor space quickly becomes a limiting factor that negatively impacts a clinic’s ability to continue to offer safe storage. Tanks become filled with abandoned embryos, leaving less room to adequately and safely inventory and manage embryos in storage for currently active patients. This “overflow” increases the chance for errors to occur as well as increases the general liability of storing large numbers of embryos. Computer records quickly become out of date and it’s difficult to keep up with all the associated data. Many records for older specimens have been sent to off-site storage, making access to this information limited. Add on top of this the growing number of oncology patients banking their tissues for extended time periods as well as more and more young career-minded women banking oocytes and/or embryos for many years and you have a storage issue that is sure to increase faster than clinics and laboratories can adapt to manage.
THE MYTH is that a clinic can provide storage for 2-5 years then require patients to find a long-term storage facility.
THE FACT is that PRIOR to beginning the IVF cycle, and the embryos going into your tanks, you have the leverage. Once the embryos are in your tank, the patient has all of the leverage. Attempting to require patients to find alternative storage years after their cycle is minimally effective. The only surefire method of preventing abandoned embryos from accumulating in your tanks is to initiate an Automatic Transfer Management (ATM) system in the beginning. Utilization of such a system requires patients to initially consent to the transfer of their embryos to a professional long-term cryostorage facility after a predetermined storage period in your facility. With Automatic Transfer Management in place, you have not only capped onsite storage needs at a manageable and sensible level, but you also benefit from third-party inventory verifications and ongoing quality assurance compliance from the professional cryostorage facility.
THE MYTH is that storing embryos is a profit center for IVF Centers.
THE FACT is only a fraction of total embryo storage fees are actually ever collected, and therefore a very small percentage of the fees find their way to your bottom line. Clinic staff have a hard time pushing collections of storage fees and/or referring patients to collections for past due storage fees due to the relationship they have built with the patient during their treatment. It is viewed as cruel to be harassing a patient for a few hundred dollars when they have paid the clinic $15,000 or more and perhaps did not even achieve pregnancy. Therefore, many of the early, and potentially effective, collections efforts are simply not completed.
Hospital-based laboratories have additional challenges. Often there is no easy interface between the laboratory to the hospital billing system. Most LIMS (Laboratory Information Management Systems) don’t allow for billing of a patient without a “visit” on record. Further, payments made by a patient to a hospital are often applied to the oldest outstanding item, which may be an emergency room visit. This can also be true in a private clinic which may be comprised of physicians of multiple OB/GYN subspecialties. So, a legitimate payment for storage fees may be recorded as a disputed patient portion of an insurance claim, thus showing a storage fee balance due when the patient is in fact paid up. This can potentially lead to the premature destruction of embryos for non-payment, now that’s a real liability.
THE MYTH is that it takes very little in the way of clinic and laboratory resources to manage embryo storage.
THE FACT is this area of management requires experience and focus. It is viewed as requiring very little time and effort simply because the jobs and tasks are often split between multiple people and tacked on to their main job descriptions as a secondary activity. However, clinic and laboratory staff are actually performing multiple time-consuming functions to service these storage accounts. When managed this way, these functions not only prove to be inefficient but a distraction from functions that could be performed by these same staff that truly deliver value to your clinic. Generally, the job of inventory management is delegated to junior laboratory personnel, and on the surface, this makes sense as they are generally lower compensated employees. However, this is a problem on many levels. First, they are more inclined to not fully understand their duties and the importance of each seemingly small task. Laboratory personnel are focused on laboratory procedures and may not see this “clerical” duty as a core duty and therefore the necessary reports which the billing department need, are often delayed, sometimes for months, and it is not uncommon to see whole years go by without storage invoicing being completed. Second, they are more likely to make errors. As we know, errors can be devastating in this business. Billing personnel often procrastinate the storage invoicing as it is not an “in-your-face” task, like setting up a patient and collecting payment for an IVF cycle or submission of insurance claims which have definite timelines. This is understandable, as those tasks are likely to bring in thousands of dollars per patient vs. a few hundred per patient when processing storage fee invoices.
THE FACT is it takes considerable time from multiple staff, each with different skills and abilities to properly perform all of the necessary functions of long-term embryo storage. Most centers lack the staff with the skill and/or time to perform these functions efficiently.