A cancer diagnosis is one of the most common reasons people will consider fertility preservation, but preservation can also be used before a military deployment, prior to a vasectomy or before people begin gender-affirming hormone replacement therapy
*American Society for Reproductive Medicine.
**American Cancer Society Facts and Figures 2020.
As you may have learned already, the cytotoxicity of chemotherapy is not limited to cancer cells. Many other cells in the body are also affected, including hair, mucosal membranes, and the germ cells that produce eggs and sperm.
Radiation Treatment:
During treatment, the prevention of pregnancy is very important, due to the risk of birth defects, stillbirths, miscarriages, or spontaneous abortions.
Although chemotherapy and ionizing radiation cause significant DNA injury, the potential for transmitting genetic defects to offspring after treatment cycles are complete is remote.
After treatment cycles are complete, no significant increase in major or minor genetic defects has been observed in the offspring of parents who have had cancer or undergone cancer therapy.
Abnormalities in sperm DNA prevent the introduction of damaged DNA into the oocyte. It is reasonable to recommend, however, that men delay attempting to father children for 6 months after completing chemotherapy or radiation therapy, to allow regeneration of developing spermatozoa.
For a more detailed breakdown of how cancer treatments impact reproductive health, please visit the National Comprehensive Cancer Network.
Military members who wish to preserve their fertility before deployment often will freeze sperm, oocytes, or embryos to safeguard their options for future family building. With active duty comes the risk of infertility for some service members. Freezing specimens before deployment will ensure your fertility is protected and is also available, with your consent, for a spouse or partner to use to achieve pregnancy while you are separated. And ReproTech offers discounted specimen storage for active-duty personnel.
Because gender-affirming hormone replacement therapy (HRT) has the possibility to negatively impact future fertility, many trans people choose to preserve and protect their fertility before beginning HRT and will work with a fertility clinic or sperm bank to freeze oocytes, embryos, or sperm for future family building.
Some programs also offer ovarian tissue or testicular tissue cryopreservation for adolescents who meet certain criteria and do not wish to do ovarian stimulation for oocyte collection or produce a sperm sample. Visit the Fertility Preservation in Pittsburgh at UPMC for more information or call them at 412-641-7475.
For sperm collection in the privacy of your home, we offer our OverNite Male kit. However, please note that sperm frozen with this kit can only be used with a sexually intimate partner, and is not meant for use as donor sperm or with a gestational carrier or surrogate in the future. If you want to use your sperm with someone who is not your sexually intimate partner or if you anticipate using a gestational carrier, please contact a fertility clinic or sperm bank to assist you with additional directed donor testing and screening.
Sperm banking is the collection, cryogenic freezing, and storage of human sperm. The sperm can be used for artificial insemination or IVF procedures for future family building.
Specimens are collected via masturbation/ejaculation either on-site at a reproductive laboratory or off-site and transported to the facility.
The most convenient, secure, private, and cost-effective method available for off-site sperm collection is ReproTech’s OverNite Male kit
Alternative collection processes include:
The total cost to freeze sperm will be dependent on the number of specimens banked as well as the facility which you use. The number of specimens required really is dependent on the sperm quality, the number of specimens, and functionality.
– Excellent pregnancy rates
– Both oocytes and sperm are needed to create embryos using a couple’s own oocytes and sperm, or with donor oocytes or donor sperm.
– Ovarian stimulation is required to increase the number of mature oocytes available for fertilization. Previously this was concerning for cancer patients who would need to delay treatment in order to freeze oocytes. New expedited stimulation protocols now allow clinics to complete oocyte retrieval faster, so fertility preservation is possible for more patients.
– Recent research shows that some breast cancer patients may be safely stimulated by tamoxifen or letrozole.
– In Vitro Maturation is another area being studied in an attempt to find methods of limited estrogen exposure.
– Cryopreservation of oocytes allows a patient to freeze their gametes for future use in creating embryos. Some patients who have a partner will freeze both oocytes and embryos so they have all options available for future family building.
– Oocyte freezing has become increasingly common for fertility preservation as vitrification has improved the post-thaw survival rates of oocytes significantly in recent years. Vitrification is the process of freezing oocytes into a glass-like state (thus avoiding crystallization) by removing water from within the oocyte and replacing it with a cryoprotective substance to prevent damage to the oocyte as it is frozen.
This procedure involves:
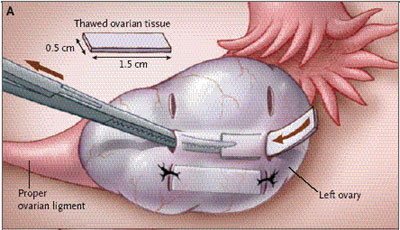
Picture of the ovarian tissue transplant procedure.
Pregnancy after Transplantation of Cryopreserved Ovarian Tissue in a Patient with Ovarian Failure after Chemotherapy, Meirow, et.al, New England Journal of Medicine, June 27, 2005, Online Content.
For the latest developments on this procedure, read more at the NCBI.
Freezing costs: $7,000-$12,000
$5,000 estimated lab & clinical services at thaw
Pregnancy rates vary between 2% to 4% per oocyte
Costs: $13,000- $25,000 – depending on whether genetic testing (PGS) and intracytoplasmic sperm injection (ICSI) is done or not.
$1,700-$2,500 estimated lab & clinical services at thaw
Pregnancy rates: 20-30% per cycle
Costs: $6,000 to $8,000, after subsidization by hospital and/or surgeon
Pregnancy rates (Limited cases, no general estimates available)

Sperm Donor
A sperm donor may be chosen by couples unable to produce children due to male infertility or by individuals without a sperm source. A donor may be chosen by the recipient (“known” donor), or recipients may choose an anonymous or non-anonymous donor via a sperm bank or agency. Pregnancy is achieved by using ART procedures. The costs of donor semen purchased from a sperm bank range at price from $200-$700 per vial. Additional insemination costs vary depending on the cycle type. Shipping and storage fees may also apply.
Egg (Oocyte) Donor
An egg (oocyte) donor may be chosen when an individual is unable to produce their own eggs (oocytes). A donor may be chosen by the recipient (“known” donor), or recipients may choose an anonymous or non-anonymous donor via an egg donation agency. The donor receives fertility medications to stimulate the production of multiple eggs. The eggs (oocytes) are then fertilized with a sperm source in a laboratory and the embryos are transferred into the recipient’s uterus. The fees paid to an egg donor and/or agency are in the $5,000-$15,000 range, with additional costs for ART procedures. Storage fees for additional embryos may also apply.
Donor Embryos
Once their family is complete, some people opt to donate excess embryos. Embryo donors complete a three-generation medical/genetic history, a psycho/social evaluation, additional blood testing, and sign an informed consent and agreement to donate. While there are many programs across the United States that administer embryo donation, there generally are waiting lists from a few months to a year or more to receive embryos. The costs to use donated embryos generally range from $2,000 to $5,000 for the above-listed embryo donor screening and legal agreements and then $2,000 to $5,000 for the frozen embryo transfer.
Gestational Carrier (Surrogate)
A gestational carrier is a person who carries a pregnancy for another person or couple. The intended parent may provide the egg (oocyte), or a donor egg used, to create the embryo, and then it is transferred to the gestational carrier’s uterus. This method is sometimes chosen when a patient has had her uterus removed, has a serious medical condition, or when recurrent IVF failure is an issue. A gestational carrier is selected through an agency or organization, with signed consent from all parties. Gestational carrier costs range from $10,000-$100,000, and costs for assisted reproductive procedures will also apply as well as storage fees. The legal status of using a gestational carrier varies by state, so it is important that a knowledgeable and reputable attorney/agency be utilized.
Oocyte vitrification for fertility preservation for both medical and nonmedical reasons
Update on fertility preservation from the Barcelona International Society for Fertility Preservation
Long-term cryostorage of semen in a human sperm bank does not affect clinical outcomes